Dr. Derek Mahony
Registered Specialist in Orthodontics
BDS(Syd) MScOrth(Lon) DOrth RCS(Edin) MDOrth RCSP(Glas) MOrth RCS(Eng)
MOrth RCS(Edin) FRCD(Can) FICD FICCDE FACD FADFE GradDipDentalSleepMedicine (WA)
49 Botany Street, Randwick NSW 2031, Sydney, Australia
Aim
Edward H. Angle dominated orthodontic armamentarium, diagnosis and treatment planning for almost a half century until Charles Tweed successfully challenged his mentor’s nonextraction mantra. The ensuing diagnostic regimen used by Tweed, however, proved to have serious limitations and clearly resulted in the extraction of too many teeth. This caused a subsequent deterioration of soft tissue appearances of patients that neither they nor their doctors liked. This article will describe and illustrate how new expansion techniques differ qualitatively from those of Angle, and how these techniques offer patients and doctors less invasive and more comfortable therapies which do not jeopardize facial appearances.
Introduction
For the first third of this past century, orthodontics found itself dominated by one man, Edward H. Angle, with the resultant intellectual stagnation that arises from such monomaniacal control. This recognition in no way detracts from Angle’s contributions – notably his clear and simple classification system along with the edgewise bracket. Both of these inventions have endured for a century, and that is no mean achievement in any scientific discipline. Nevertheless, orthodontists’ unquestioning acceptance of his limited diagnostic and treatment planning regimens hindered the advancement of this discipline more than it helped, and the last half of this past century was spent trying to overcome the stupor of the first half.
Angle’s influence continued until an apostate student of his, Charles H. Tweed,[1] had enough courage and objectivity to challenge Angle’s non-extraction scheme. It wasn’t a tremendous leap of intellectual power. Tweed simply and honestly recognized that when 100% of your patients relapsed, there might be something wrong with the diagnosis and/or treatment planning.
Dr. Tweed acted appropriately in the face of this challenge – quite unlike the ancient dentist who chided a young colleague who was describing his meticulous technique of endodontic filling to the monthly assembly of dentists. The old man explained his own technique that used a simple matchstick sharpened with a pocketknife and then jammed into the canal. When the young dentist asked if a lot of these root canal fillings didn’t subsequently fail, the older man replied, “Every damn time!”
Dr. Tweed tired of those orthodontic abscesses and, unlike his peers, sought to correct the deficiencies he saw in Angle’s philosophy. Some would say that he overcorrected, but that said, we must pay homage to anyone who has the skill and temerity to successfully challenge a mentor and his minions. Tweed’s success brings to mind the remark of C.S. Lewis, who said, “No genius is so fortunate as he who has the skill and ability to do well that which others have been doing poorly.”
Nevertheless, I don’t think that Tweed would have ever been able to deliver his paper describing his extraction technique had Dr. Angle still been alive. Angles influence over the society that bore his name was too immense to permit such hubris from a young upstart. But as Samuelson, the MIT economist, once noted: “Science progresses slowly – funeral by funeral.” And so it was and is in orthodontics.
Nonextraction Philosophy
Aside from the edgewise bracket and the classification system, Angle’s most enduring legacy has been his belief in nonextraction therapy. Angle had unsuccessfully experimented with premolar extractions while using his ribbon arch appliance, but he never solved the problem of paralleling the roots to prevent the extraction spaces from opening. If he couldn’t do it, then, ergo, no one else could, and this resulted in a virulent opposition to any extractions and an insistence upon enlarging the arches to accommodate all of the teeth.
This dogma stayed dominant for several decades until Tweed advocated the extraction of premolars based on his diagnostic triangle, which was the first systematic treatment planning stratagem orthodontists had. Tweed received corroboration simultaneously from another former Angle protégé in Australia, Raymond Begg,[2] who had studied aborigines and concluded that nature intended for enamel to wear. He decided that orthodontists could mimic nature by extracting teeth prior to orthodontic therapy. The Tweed and Begg Extraction Philosophies eventually prevailed and remained uncontested for some time.
Several years past before Holdaway[3, 4] published his articles that suggested the soft tissue as the determining feature of diagnosis. This disputed Tweed’s narrow diagnostic regimen that focused on the mandibular incisor and totally neglected the soft tissue. Tweed’s triangle set in motion a trend that emphasized more prudence in the extraction of teeth. Soon others added their discoveries regarding soft tissue and the maxillary incisors as main determinants of diagnosis and treatment planning.[5-7]
From the inception of this specialty, with Dr. Angle, diagnosis never had too much importance because everyone received the same nonextraction treatment with the same expansive appliance. The marvel of it all is that the collection of orthodontic records never became important. A few months ago an orthodontist boasted that since invoking a different treatment regimen, he was treating 98% of his patient’s nonextraction. One was tempted to ask if he still took records because with diagnostic certainty such as that, records are clearly redundant. Orthodontists shouldn’t waste patients’ time and money taking impressions, cephalometric X-rays or doing treatment simulations if all treatment plans are essentially the same. One doesn’t need orthodontic records to come to such a preconceived conclusion.
Obviously, this one-size-fits-all treatment planning didn’t benefit patients a hundred years ago, and it doesn’t in our own age. But such simplicity continues to hold enormous appeal for many orthodontists. Orthodontists pride themselves in being scientists, and without doubt they receive good training in the scientific method; but it takes very little anecdotal information to eclipse the scientific judgment of many in the profession. Albert Szent-Györgyi was probably more right than he knew when he said, “The brain is not an organ of thinking but an organ of survival like a claw and fang. It is made is such a way as to make us accept as truth that which is only advantage.”
No matter how spectacularly orthodontic therapy changes, it will benefit our patients minimally if we do not have a concomitant improvement in our diagnostic and prognostic knowledge. This remains the number one imperative for those who practice orthodontics. Orthodontists should view any new therapy unaccompanied by equally sophisticated diagnostic knowledge suspiciously. Patients have already received far too much orthodontic treatment and far too little diagnosis.
Instrumentation
The first attempts to correct malocclusions used simple large arch wires ligated to the malposed teeth. Pierre Fauchard of France developed the precursor of the modern appliance – expansion arch (Figure 1).
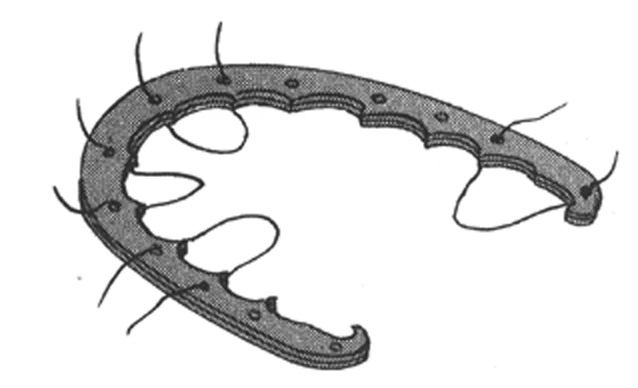
Figure 1: Fauchard’s expansion arch
This arrangement gave only tipping control, in one dimension, and soon proved inadequate for controlling rotations. In 1887 Edward H. Angle introduced the E arch, i.e. expansion arch that used a labial wire supported by clamp bands on the molar teeth which ligated to the other teeth (Figure 2).
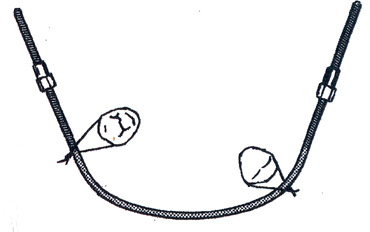
Figure 2: Angle’s E Arch
Metallurgical developments by the early 20th Century allowed clinicians to encase all of the teeth with bands and solder attachments that could control the horizontal rotations. Angle developed a popular attachment known as the pin and tube attachment in 1911 (Figure 3), and it satisfied many of the requirements of clinicians; but this demanded unusual dexterity, patience and skill, so dental clinicians evolved to a ribbon arch bracket (Figure 4), which Angle introduced in 1916. It provided good control in two dimensions and became popular quickly. The ribbon arch attachment also marked the first time orthodontic attachments gained the name bracket.[8]
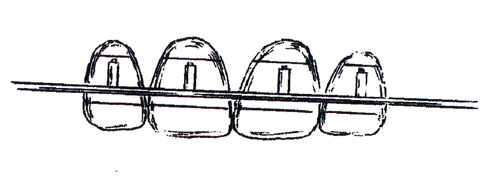
Figure 3: Pin and tube appliance
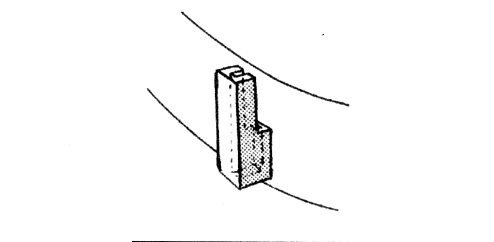
Figure 4: Ribbon arch
When Angle launched the ribbon arch bracket, he had already started work on the edgewise bracket primarily as a supplement to his ribbon arch appliance. Nevertheless, the edgewise bracket did not suddenly spring full-grown from Angle’s fertile mind, but slowly evolved with several iterations (Figure 5). When Angle realized that this bracket could deliver three-dimensional control of the teeth with horizontal, one directional placement and simultaneous engagement of all the teeth, he changed the bracket several times until he achieved the #447 (Figure 6) in 1928. It received early and enthusiastic endorsement from dental clinicians throughout the United States and eventually eclipsed other useful orthodontic appliances such as the McCoy open tube appliance, the Atkinson universal appliance and the Johnson twin wire attachment.
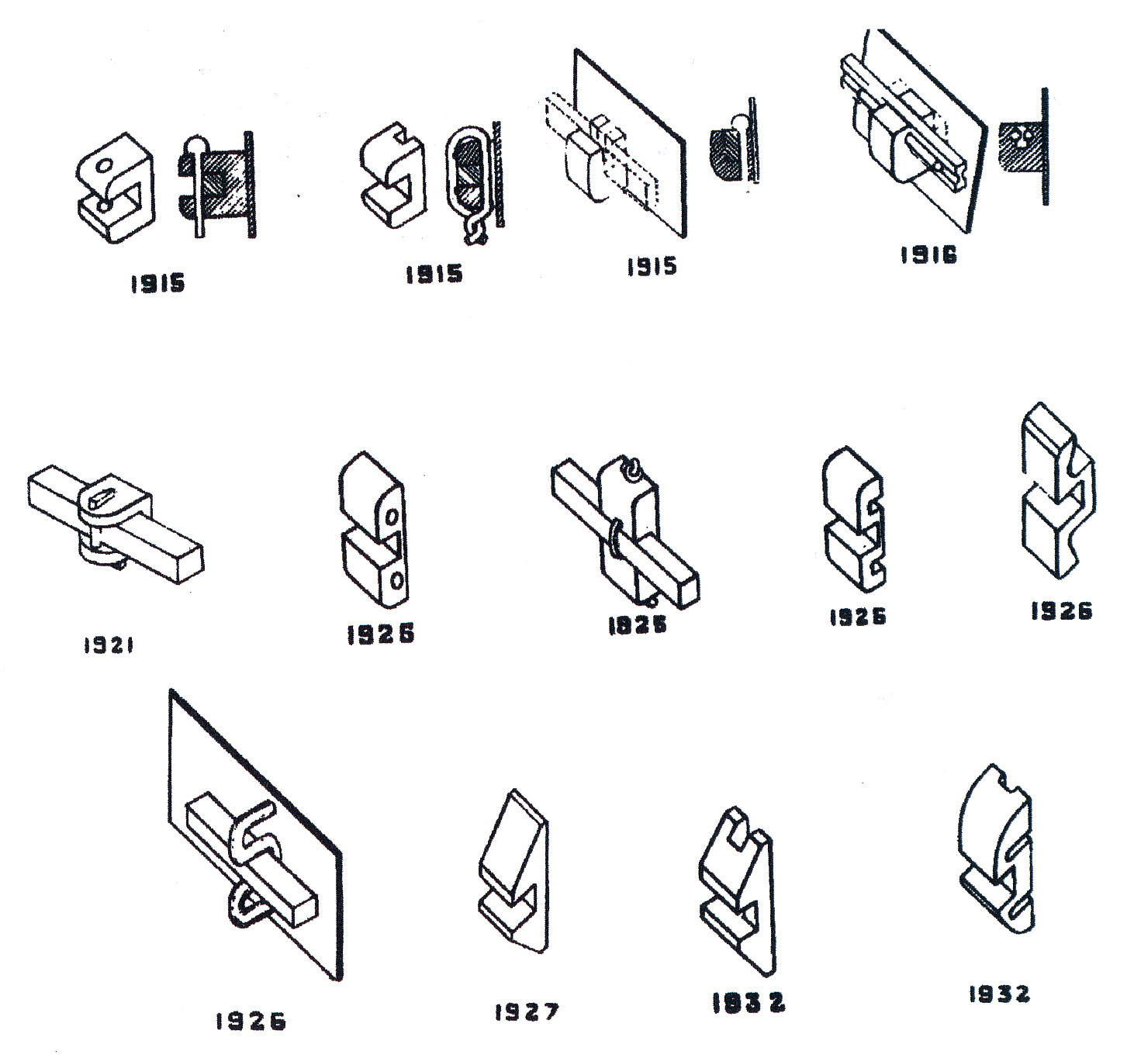
Figure 5: Angle’s many iterations of the edgewise bracket
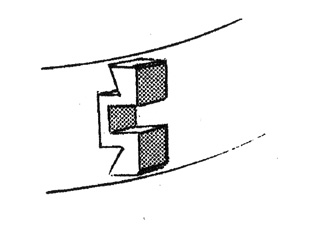 Figure 6: Angle’s 447 edgewise bracket, “the latest and best in orthodontic mechanisms.”
Figure 6: Angle’s 447 edgewise bracket, “the latest and best in orthodontic mechanisms.”
The universal application and durability of the edgewise bracket confirmed Angle’s immodest claim that it offered the “latest and best in orthodontic mechanisms”.[9] Innovators have added minor but practical trimmings such as rotating wings, twin brackets, different dimensions, preadjusted appliances, lingual applications, etc., but the essence has remained edgewise. For any instrument, particularly in the health sciences, to remain virtually unchanged (and almost as useful for close to a century) approaches unbelievability. In the automobile industry, this would be equivalent to the Model T Ford remaining as the epitome of motoring sophistication.
Other than adding wings and doubling the bracket to make the popular twin edgewise bracket, Angle’s invention has remained basically unchanged. Holdaway[10] suggested angulations for brackets to help set anchorage, parallel roots and artistically position teeth, while Lee[11] had built some anterior brackets with the ability to torque incisors. But it was Andrews that was to develop an appliance that would apply 1st, 2nd and 3rd order movements to the teeth without making changes in the wire – hence the Straight Wire Appliance.[12]
Preadjusted orthodontic appliances have dominated the profession for the past 30 years, and the belief in them shows little sign of abating even though many have questioned the one-size-fits-all idea.[13-18]
And Back Again
The publication of Frankel’s[19] work with functional appliances illustrated significant enlargement of dental arches and reawakened an interest in nonextraction therapy. Nevertheless, Frankel mechanics required the use of removable appliances, and that didn’t resonate well with many orthodontists or their patients. After a brief flurry of interest in the United States, few clinicians continued to use the Frankel appliance on a regular basis.
Nevertheless, the successful use of orthopedic appliances alerted orthodontists to the possibility of increasing arch widths and arch perimeters with minimum forces. Although mandibular canines offer significant resistance to expansion, mandibular premolars and first molars often demonstrate substantial and stable expansion. Brader[20] hinted at this with his work on the tri-focal ellipse arch form, but he didn’t follow through about how this might give wider and more accommodating arch forms.
Low-force titanium coil expanders have shown their ability to develop arches laterally,[21] and recently Damon[22] has suggested that low arch wire forces, coupled with a passive tube and a small wire-to-lumen ratio, enable teeth and their accompanying dentoalveoli to expand in all planes of space. Damon feels that using small, low-force wires such as those of Copper Ni-Ti™ (Ormco Corporation, Orange, CA) achieves the ideal biological forces proposed long ago by several investigators.[23] [24, 25]
Self-ligating brackets that essentially form a tube developed several decades ago with the Ormco Edgelok[26] being the first, closely followed by the Speed bracket[27]. Both of these early self-ligating systems suffered from the fact that the Straight-Wire Appliance phenomenon debuted at the approximately the same time, plus a lack of appreciation for what the newer titanium wires could achieve.
Damon has persisted since 1995 with his version of a self-ligating bracket (Figure 8) and has fundamentally changed the types of arch wires and the sequence in which clinicians use them. His experience has shown that with many patients he can often eliminate distalisation of molars, extractions (excluding those needed to reduce bimaxillary protrusions) and rapid palatal expansion. He offers compelling clinical evidence of doing this with consistency. [22]
The Damon bracket is essentially a tube designed with the right dimensions to foster sliding mechanics where needed and enough play in the system for torque and rotational control using the larger cross section wires. Damon starts cases with a large lumen arch wire slot and .014 or smaller diameter hi-technology arch wires. Starting cases with a large dimension passive arch wire slot and small diameter wires diminishes the divergence of the angles of the slots. This lowers the applied force and binding friction. (figure 7)
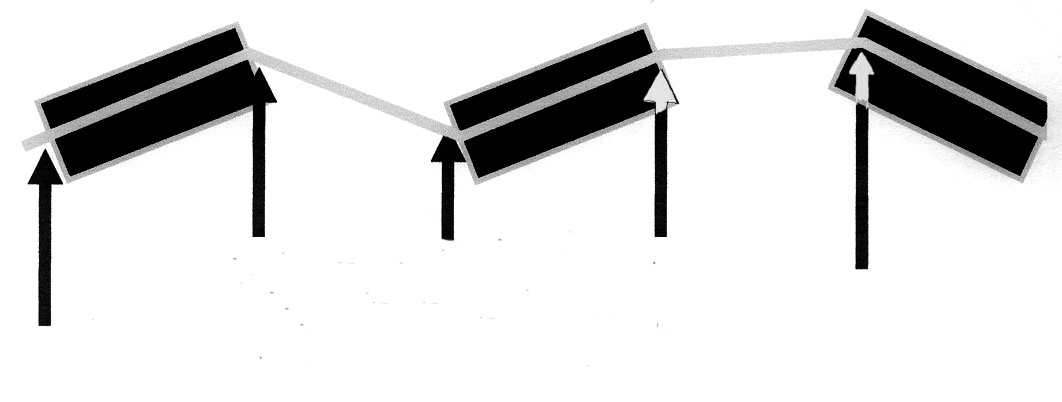
Fig 7a: Binding
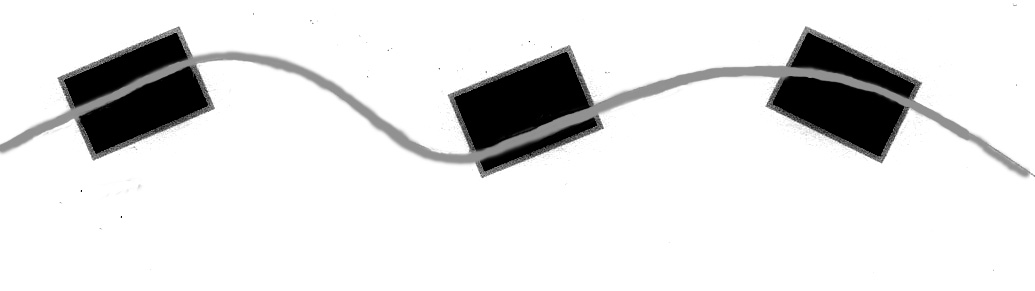 Fig 7b: Divergence
Fig 7b: Divergence
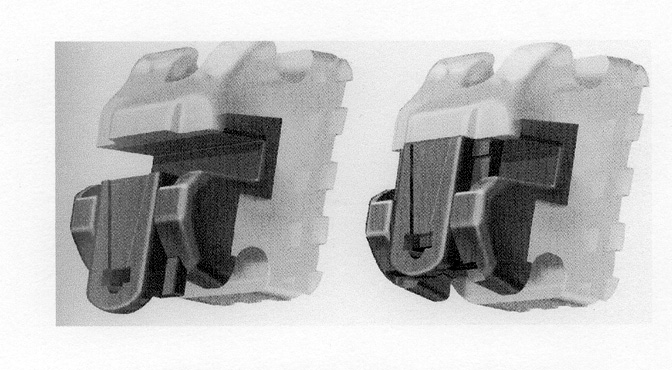
Figure 8: Damon 3 bracket opened and closed
The most logical questions readers could propose would be why has Damon shown successful expansion whereas Angle did not? The quantity of expansion probably differs little, but the quality of expansion offers a quantum change. Mollenhauer[28] has suggested as much with his appeal for light forces. Even though Angle used a ribbon arch, (which suggests a thin, delicate wire) the actual size of the wire had the dimension of .036 x .022 inches. Ligating to this wire would overwhelm the periodontium and prevent the development of a supporting dentoalveolus. Rather than forming new bone, the supporting dentoalveolus would simply bend and upon completion of treatment quickly return. Astute clinicians often see this with molar distalization from headgear use and over treat such movement in order to compensate for this regressive bone bending.
Schwartz [25] stated that it takes 20 to 26 g/cm² of force to collapse the capillaries in the Periodontal Ligament. With RPEs and headgears this force sometimes exceeds 10 pounds!
Profitt [29] states that that optimal force levels for orthodontic tooth movement should be just high enough to stimulate cellular activity without completely occluding blood vessels in the periodontal ligament.
True Biomechanics is staying in the Optimal Force Zone i.e. keeping forces below capillary blood pressure. Conventional ties (o-rings and stainless steel ligatures and spring clips) make staying in the Optimal Force Zone nearly impossible due to the increased binding and friction.
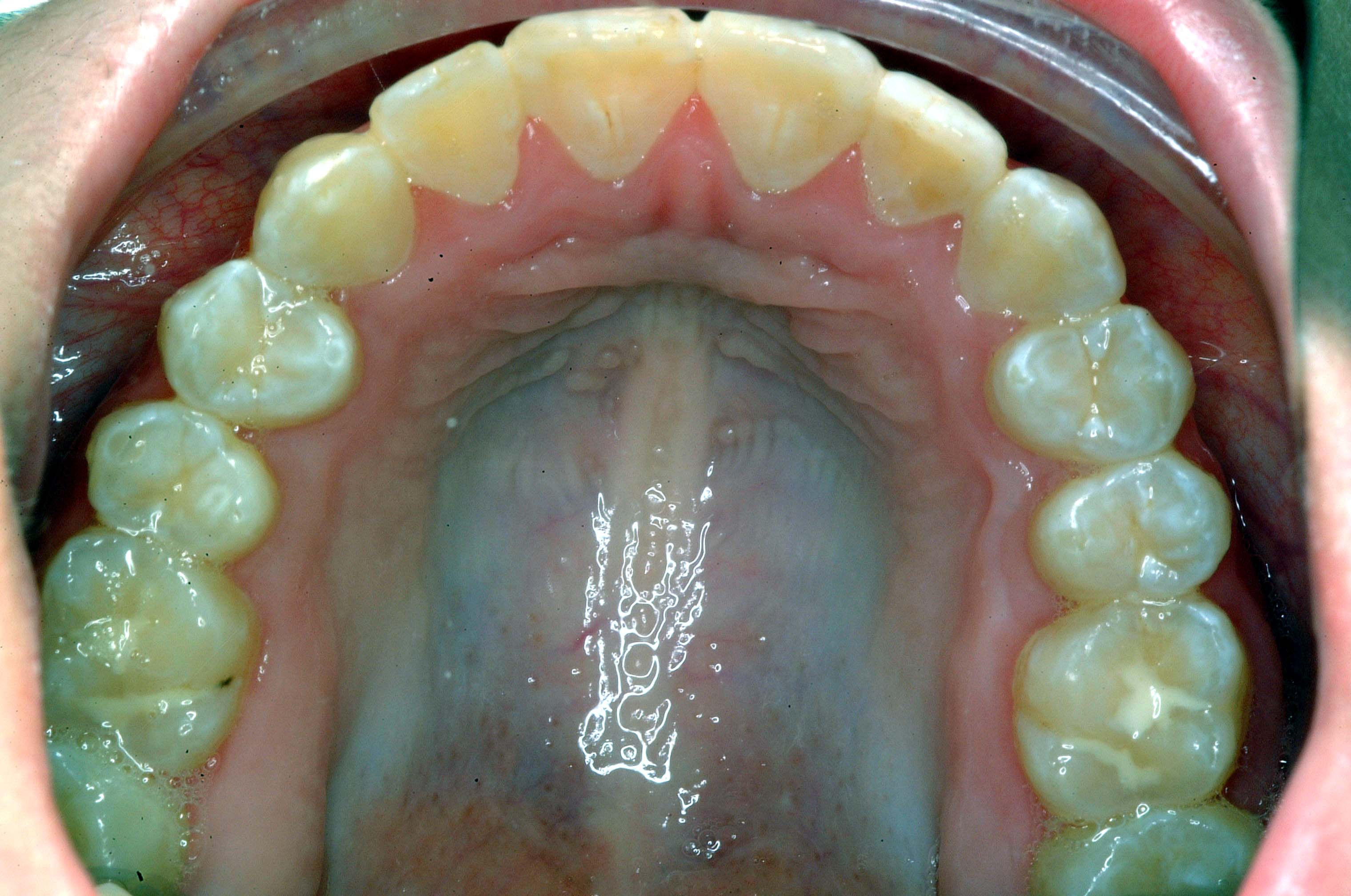
The most important caveat Damon offers clinicians is not to use their ordinary mechanics with his system, and I could not agree more. When I first began to use the Damon system, I continued to use the regular sequence of arch wires and saw little advantage to these new, more expensive brackets. Nevertheless, as I began to use the brackets according to Dr. Damon’s advice, I started seeing phenomenonal changes. The following patient illustrates typical responses to the biomechanics offered by the Damon System:





Summary
The paradigm shift in our current thought processes is the belief that alveolar bone can be altered and re-shaped with low clinical forces. Using low force, low friction orthodontics, the alveolar bone allows the bodily movement of teeth in all directions.
The architecture of alveolar bone appears to improve over time following low force orthodontics so clinicians should be very creative on how to maintain the appropriate biologic forces during all phases of treatment.
Orthodontists are currently witnessing an interest in qualitatively different expansive biomechanics that offer patients the possibility of obviating the use of distalizers, rapid palatal expanders and many needless extractions. The bracket systems that make this possible should command the utmost respect and clinicians should use them as recommended with light forces.
I am witnessing shorter treatment in most of my Damon cases with less discomfort to my patients. The playing field seems to be leveled between adults and children. These changes I am seeing are more than enough reasons for me to question my previous force systems.
- Tweed, C.H., The Frankfort mandibular incisor angle (FMIA) in orthodontic diagnosis, treatment planning and prognosis. Angle Orthod, 1954. 24: p. 121-169.
- Begg, R., Begg orthodontic theory and technique. 3rd ed. 1977, Philadelphia: W.B. Saunders Co.
- Holdaway, R.H., op. cit., A soft tissue cephalometric analysis and its use in orthodontic treatment planning, Part II. Am. J. Orthod., 1984. 85(4): p. 279-293.
- Holdaway, R.H., A soft tissue cephalometric analysis and its use in orthodontic treatment planning, Part I. Am. J. Orthod., 1983. 84(1): p. 1-28.
- Alvarez, A., The A Line: A New Guide for Diagnosis and Treatment Planning. J. Clin. Orthod, 2001. 35(9): p. 556-569.
- Creekmore, T.M., Where teeth belong and how to get them there, J. Clin. Orthod, 1997. 30(9): p. 586-608.
- Sarver, D.M., Profitt, W.R., Special Considerations in Diagnosis and Treatment Planning. 4th ed. Orthodontics – Current Principles and Techniques, ed. Tom Graber. 2005, St. Louis, MO: Elsevier Mosby. 1213.
- Renfroe, E.W., Technique Training in Orthodontics. 1st ed. 1960, Ann Arbor, MI: Edwards Brothers Inc. 230.
- Angle, E.H., The latest and best in orthodontic mechanism. Dental Cosmos, 1929. 71: p. 164-174, 260-270, 409-421.
- Holdaway, R.A., Bracket angulation as applied to the edgewise appliance. Angle Orthod, 1952. 22: p. 227-236.
- Lee, I.F.
- Andrews, L.F., Straight Wire, the Concept and Appliance. 1989, San Diego, CA: L.A. Wells Company.
- Andreiko, C., JCO interviews Craig Andreiko, DDS, MS, on the Elan and Orthos Systems. J. Clin. Orthod, 1994. 28(August): p. 459-472.
- Sachdeva, R., SureSmile technology in a patient-centered orthodontic practice. J. Clin. Orthod., 2001. 35(April): p. 245-253.
- Melsen, B.F., Giorgio, Biomechanics in Orthodontics, Libra Ortodonzia.
- Creekmore, T.C., R., Straight Wire: The Next Generation. Am J.Orthod & Dentofacial Orthop, 1983. 104(July): p. 8-20.
- Dellinger, E.L., A scientific assessment of the straight-wire appliance. Am J Orthod, 1978. 73: p. 290-299.
- McGann, B.D., Individual patient (IP) appliances. World J. Orthod, 2005. 6(2): p. 189-192.
- Frankel, R., The Frankel Appliance (The Function Corrector(Removable Orthodontic Appliances, ed. T.G. Neumann. 1977, Philadelphia, Pa: W. B. Saunders Company.
- Brader, Dental arch form related with intraoral forces: PR=C. Am. J. Orthod., 1972. 61(June): p. 541-561.
- Williams, M.O., White, L.W., A Rationale for Expansion. World J. Orthod, Pending Publication.
- Damon, D.H., Treatment of the face with biocompatible orthodontics. 4th ed. Orthodontics – Current Principles and Techniques, ed. Tom Graber. 2005, St. Louis, MO: Elsevier Mosby. 1213.
- Reitan, K., Tissue behavior during orthodontic tooth movement. Am J Orthod, 1960. 46: p. 881-900.
- Rygh, P., Elimination of hyalinized periodontal tissues associated with orthodontic tooth movement. Scand J Dent Res, 1973. 81: p. 467-480.
- Schwartz, A.M., Tissue changes incidental to orthodontic tooth movement. Int J Orthod Oral Surg Radiography, 1932. 18: p. 331.
- Wildman, A.J., Lee, I.F., Hice, T.L., Lang, H.M., Strauch, E.C. Jr., The Edgelok Bracket. J Clin Orthod, 1972. 6(11): p. 613-633.
- Hanson, H., Dr. G. Herbert Hanson on the Speed Bracket. J. Clin. Orthod., 1986. 20(3): p. 183-189.
- Mollenhauer, B., Ultralight forces for simultaneous orthodontics and orthopedics: part III. dentofacial orthopedics. World J. Orthod, 2000. 1: p. 195-201.
- Proffit and Fields, Contemporary Orthodontics, Second edition, Mosby 1993