Unique site-specific factors control oral immunity
The body’s barrier sites, such as the skin, mouth and intestines, are continually exposed to potentially harmful foreign substances and infectious agents, and they are also home to a diverse array of harmless microbes called commensal microorganisms. Oral immunity is dependent on the immune system performing a remarkable balancing act at these sites by fighting off dangerous pathogens while tolerating the presence of the normal flora.
Multiple cell types are involved in protecting the body’s barriers, including immune cells called Th17 cells. These cells have been shown to help assist oral immunity and combat infections in the oral cavity—people with genetic defects in Th17 cell function experience frequent fungal infections of the mouth. Conversely, exaggerated Th17 cell responses have been linked to periodontal disease, underscoring the importance of precise control of the cells’ function. Previous research has shown that certain microbes regulate Th17 cells in the skin and intestines, but the factors that control them in the mouth have been less clear.
Niki M. Moutsopoulos, D.D.S., Ph.D., chief of the Oral Immunity and Infection Unit at the NIH’s National Institute of Dental and Craniofacial Research (NIDCR), wondered if, similar to other barrier sites, microbes control Th17 cell accumulation in the mouth.
Dr. Moutsopoulos has a longstanding interest in how microorganisms and the immune system interact to preserve the health of the oral cavity. Her research team focuses on the molecular pathways that lead to periodontal disease, with the ultimate goal being to identify therapeutic targets for this common condition.
In the current study, which was published in the journal, Immunity, and was carried out in collaboration with Joanne E. Konkel, Ph.D., of the University of Manchester, the researchers observed that Th17 cells appear in the oral cavity with age. There were few Th17 cells in young, 8-week-old mice but by 24 weeks, middle age for mice, Th17 cell numbers had increased dramatically. Based upon what was known about Th17 cells in the skin and intestines, the researchers suspected that the cells’ surge in middle age might involve shifts in microbial populations.
To their surprise, they found that the composition and levels of microbes in the oral cavity of 8-week-old mice were comparable to those of the 24-week-old mice. In addition, mice raised in a germ-free environment had similar oral Th17 cell levels as mice raised under normal, non-sterile conditions. These findings revealed that, in contrast to other barrier sites, the presence of Th17 cells in the mouth does not depend on microbes. The researchers concluded that factors that regulate Th17 cells must differ depending on the unique characteristics of each site.
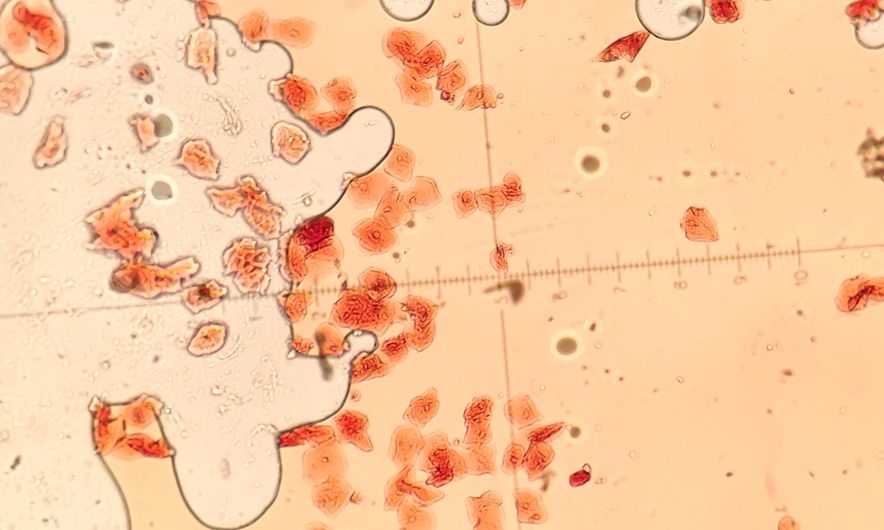
Th17 cells are key mediators of immunity at barrier sites such as the oral cavity. The factors that control them differ depending on cues unique to each site’s local environment. Credit: Niki M. Moutsopoulos, D.D.S., Ph.D., NIDCR.
A clue as to what these factors might be in the oral cavity came from experiments showing that a signaling molecule called IL-6 is needed for Th17 cell accumulation—mice engineered to lack IL-6 produced far fewer Th17 cells compared to control mice that have the molecule. Dr. Moutsopoulos’s team next focused on identifying the factors that induce IL-6 and drive Th17 cell accumulation at this barrier. They hypothesized that “damage signals” caused by chewing could stimulate the local immune response.
Subsequent experiments validated this idea. The researchers found that mice raised on a soft food diet requiring minimal chewing had fewer Th17 cells by 24 weeks than mice fed a normal diet. In addition, Th17 cell numbers rose in the mouths of young mice when the researchers hardened the diet or induced damage by mechanical abrasion. This rise in Th17 cell levels did not occur in mice lacking IL-6, confirming the key role of this signaling molecule in promoting Th17 cell accumulation.
Together, these findings have uncovered a role for mechanical damage in triggering local immunity in the oral cavity, and have linked induction of Th17 cells to the stimulation of protective immune responses. However, exaggeration of these signals could be pathogenic and contribute to inflammation and periodontal bone loss.
“We know that Th17 cells are important for preserving the health of the oral cavity, but they also may contribute to periodontal disease, which is why we want to understand the factors that regulate them in this unique environment,” said Dr. Moutsopoulos.
More generally, the findings highlight the importance of evaluating the local environment for novel factors that may control immune responses at barrier sites.
This study was funded in part by the intramural program of NIDCR, the Biotechnology and Biological Sciences Research Council, the Wellcome Trust and the Manchester Collaborative Centre for Inflammation Research.
On-going mechanical damage from mastication drives homeostatic Th17 responses at the oral barrier. Dutzan N, Abusleme L, Bridgeman H, Greenwell-Wild T, Zangerle-Murray T, Fife ME, Bouladoux N, Linley H, Brenchley L, Wemyss K, Calderon G, Hong B, Break TJ, Bowdish DME, Lionakis MS, Jones SA, Trinchieri G, Diaz PI, Belkaid Y, Konkel JE, and Moutsopoulos NM. Immunity. 2017 Jan 6. doi: 10.1016/j.immuni.2016.12.010. [Epub ahead of print] PMID: 28087239