Dr. Derek Mahony
Registered Specialist in Orthodontics
BDS(Syd) MScOrth(Lon) DOrth RCS(Edin) MDOrth RCSP(Glas) MOrth RCS(Eng)
MOrth RCS(Edin) FRCD(Can) FICD FICCDE FACD FADFE GradDipDentalSleepMedicine (WA)
Summary
Overclosure is a common condition among patients seeking restorative and/or orthodontic rehabilitation. By evaluating the patient for common signs and symptoms associated with overclosure, one can determine the need for re-establishing a physiologic vertical dimension. Opening of the bite can be accomplished in a number of ways by following specific guidelines. The use of objective diagnostic aids are extremely helpful by allowing the clinician to optimize TMJ and craniofacial muscle function at the new VDO. The correction of the vertical dimension during a rehabilitative procedure should result in enhanced comfort and improved function in the finished case.
Introduction
The term neuromuscular occlusion has become associated with certain limited methodologies that are used to obtain a muscle-compatible occlusal relationship. In reality, there are several different approaches that can be used to determine a “neuromuscular” maxillo-mandibular relationship, even with a fully edentulous case. Within each method, however, the common basis for all muscle-oriented approaches involves first determining the resting length of the masticatory muscles.
Historically, opening the bite has been considered hazardous and/or foolhardy by many dentists and with good reason. Arbitrary opening of the bite, especially when accomplished strictly on an articulator, can result in a difficult, uncomfortable and unappreciative patient. Some dentists have recommended against ever opening a bite, perhaps after an especially troublesome experience with a patient.
In spite of the risks, there are some advantages associated with opening an over-closed bite. The identification can be traced back at least 70 years to an ENT physician, Dr. J. B. Costen.1-3 Dr. Costen discovered, perhaps quite by accident after referring many of his symptomatic, edentulous patients to a local dentist for new dentures, that many returned with their head and ear pain symptoms greatly relieved. His publications were positively received at the time and, in fact, what we refer to today as temporomandibular disorders (TMDs) were originally referred to as “Costen’s Syndrome.” While we know today that many TMD patients are not over-closed, over-closed patients do often exhibit some of the signs and symptoms commonly associated with TMD. Thus, although over-closure in and of itself is not pathognomonic of TMD, it should be considered as a risk factor.
The use of the patient’s own muscles to determine the vertical dimension of occlusion was already being explored in the 1940s by people like orthodontist John R. Thompson.4 Sears5 introduced the concept of the “Pivot Appliance” in the 1950s, which was designed to open the bite enough to allow the patient’s muscles to reposition the mandible. Following their lead, others6-28 have subsequently evolved the current array of neuromuscular registration methods presently in use. At the same time several studies29-32 have demonstrated that a muscle-determined position, although similar, is not identical to centric relation.
Common signs and symptoms of over-closure
When asked, over-closed patients often report symptoms such as frequent headaches, dull pain of the elevator muscles and pain or stiffness in their neck muscles. Ear stuffiness, tinnitus and/or vertigo are also commonly reported. A more subtle symptom, less often reported, is frequent gastrointestinal distress in various forms that has no clear, identifiable cause. This may also be accompanied by a report of difficulty in chewing and/or swallowing. An overclosed patient will usually report several, but not all, of the following symptoms:
- Frequent headaches with no identifiable cause
- Ear stuffiness with no indication of ear pathology
- Difficulty in chewing tough foods
- Difficulty or discomfort in swallowing
- Frequent gastrointestinal distress
- Vertigo
- Tinnitus
- Persistent dull pain in masticatory elevator muscles
- Neck pain or stiffness
- Possible increased wear of incisor teeth
Under examination, a number of signs indicating over-closure may appear. These include; 1) a measured freeway space greater than 3 mm, 2) EMG or visual identification of a tongue-thrust swallow, 3) the appearance of less than fully erupted molars, 4) a deep curve of Spee, 5) one or more posterior edentulous spaces, 6) lingually tipped mandibular molars, 7) EMG identification of elevator muscle hyperactivity at rest of more than 2.0 microvolts average (or 2.2 microvolts RMS), 8) worn and shortened teeth (there is no scientific evidence that human teeth “grow out” in response to wear in the way that elephant’s teeth do), 9) horizontal skin creasing and saliva weeping at the corners of the mouth, 10) a so-called “Shimbashi” measurement (in centric occlusion) of less than 16 mm from the cemento-enamel junction of the maxillary central incisor to the cemento-enamel junction of its opposing mandibular tooth and 11) long-term chronic internal derangement of the TM Joint(s). However, patients rarely seek dental treatment for any of these objective signs. Instead, they are more likely to seek rehabilitative treatment for headache, jaw-ache, ear-ache, difficulty in chewing/swallowing or for purely aesthetic reasons. In other cases, they are unaware of their condition, apparently due to their excellent adaptability. In the over-closed patient, the “reason” for treatment either cosmetic or functional, is often dependent more on his/her individual adaptability than on the dental conditions present. While some signs simply indicate the “progress of the destruction” that a pathological maxillo-mandibular relationship fosters, other signs may indicate a successful adaptation.
- Freeway space > 3 mm [if pain level is low, it is an adaptation, otherwise it is not]
- Tongue thrust swallow [if full arch tongue thrust, usually a successful compensation]
- The appearance of less than fully erupted molars [tongue inhibition of natural eruption]
- A deep curve of Spee [often associated with one or more missing molars or a deep anterior overbite with retroclined upper incisors]
- One or more posterior edentulous spaces [leads to deep curve of Spee]
- Lingually tipped posterior teeth [tongue thrust during swallow, restricted maxillary arch]
- Hyperactivity of elevator muscles at “rest.” [an adaptation, successful if no elevator muscle pain]
- Worn/short teeth, abfractions (ground off) [not a successful adaptation]
- Skin creasing at corners of mouth [may appear as aesthetic problem only, not an adaptation]
- Saliva weeping at corners of mouth [an aesthetic and functional problem, not an adaptation]
- CEJ (cemento-enamel junction) to CEJ in C.O. < 16 mm. [less than the normal adaptive range]
- Internal derangement(s) of the TMJ [if no degeneration, may be a successful adaptation]
Maxillo-mandibular bite relationships
Centric occlusion (CO = habitual)
The maxillo-mandibular position of maximum intercuspation is most often the dental treatment position, primarily by default. This is of necessity whenever single tooth preparations or small restorations are involved, since they must fit within the patients existing occlusal scheme. It is only at times of major reconstructive, orthodontic and/or surgical treatments that the option of opening a bite or establishing a new maxillo-mandibular relation may present itself. However, many clinicians still prefer to “play it safe” and retain the existing habitual (CO) maxillo-mandibular relationship, even during major rehabilitative procedures. By definition, the use of centric occlusion as a treatment position excludes re-establishing a proper vertical dimension in an over-closed patient. However, if the patient’s condition is actively deteriorating this may not be a safe option at all, as the continued physiologic breakdown may lead to failed dentistry and/or a flair up of craniofacial pain.
Centric relation (CR)
The concept of centric relation has a very long history and was originally devised, at least in part, to accommodate the use of articulators during prosthodontic treatment. Although we now know that the jaw doesn’t function like a hinge, originally it was convenient to make that assumption when using articulators to make prostheses. Today, one clear difference between centric relation procedures and strictly muscle-oriented methodologies is the priority given by CR methods to evaluating the function of the temporomandibular joints. Typically, centric relation operators give first priority to establishing stable joint function, while muscle-oriented (neuromuscular) approaches tend to focus almost exclusively on muscle comfort.
Muscle-related centric (MC)

Figure 1. BioJVA testing for normal TM joints
In general, muscle-oriented approaches consider joint position and/or stability secondary to muscle function. In the extreme, it is simply assumed that creating “happy muscles” will automatically provide good or at least adequate joint function. In a more practical view, both joint function and muscle function are seriously evaluated and, when indicated, a compromise is sought to provide both joint and muscle compatibility. This represents an approach that bridges the gap between strict CR and rigid MC approaches. Consequently, a variety of methods have evolved to capture and establish a muscle-related centric position, while maintaining favourable joint function.
The requirements of proper neuromuscular occlusion (NMO)

Figure 2. Bio-TENS, a ULF-TENS unit used for muscle relaxation
The first step in all approaches to NMO requires inducing relaxation in the masticatory musculature, however, there is no rational excuse for not evaluating TM joint function prior to beginning the process. This can be accomplished quickly and easily with Joint Vibration Analysis (JVA see figure 1.), or with more expensive and invasive imaging such as MRI. Muscle relaxation can be aided by Ultra-Low Frequency TENS (ULF-TENS, see Figure 2.), an Aqualizer, soft music or any other technique that reduces the resting hyperactivity of the masticatory muscles.
Surface electromyography (see Figure 3.) is useful for making a quantitative determination whether relaxation has occurred or whether resting muscle hyperactivity still exists. Needles and/or fine wire electrodes not only make relaxation less likely, they record a more localized signal that is less representative of overall muscle activity. However, needle EMG electrodes are required when one is seeking to differentiate a myopathy from a neuropathy. Using the relaxed rest position of the mandible, with respect to the maxilla as a reference, a clinician can select a vertical dimension that allows adequate freeway space, yet avoids over-closing the bite. There are several methods currently used for selecting the treatment vertical. Each has its own rationale and advantages, but all of them benefit from objective diagnostic aids to ensure the best compromise between optimum joint, muscle, and tooth function.

Figure 3. BioEMG II for monitoring rest position and testing muscle function against the new bite
Several muscle-oriented bite registration techniques
The wax swallow bite registration
A physiologic, muscle-oriented, vertical dimension can be obtained by means of the swallowing reflex technique originally proposed by the late Dr. Willie May. Currently, the wax swallow bite technique, developed by James Carlson, is a simple, direct close approximation of a muscle-related bite registration. Small pillars of soft wax are placed on the first molars, then the patient is instructed to swallow several times. Subsequently, fast-curing impression material is injected around the arch to firmly establish the maxillo-mandibular relationship. Since humans swallow thousands of times per day, it has been proposed that the swallow position should be compatible with the musculature. This technique is recommended only after verification of good TM joint function with Joint Vibration Analysis or MRI.
The ULF-TENS bite registration
Ultra-low Frequency TENS, originally conceived by Bernard Jankelson, is often used to relax the masticatory muscles. It can also be used to determine a bite registration position, sometimes referred to as myo-centric. After a patient has been “pulsed” for relaxation, usually for about 40 minutes, bite registration material (a quick-cure acrylic) is placed over the mandibular occlusal surfaces and the ULF-TENS is re-applied to “close” the mandible about 1 – 2 mm above the rest position. During this procedure the vertical dimension is usually monitored with a mechanic’s inside callipers between marks on the chin and nose. There is a definite “technique sensitivity” to this procedure such that different operators tend to produce slightly to greatly different results. However, once the skill is developed, an operator may produce good consistency. These classic TENS bites ignored the TM joints function in the past, but this should no longer be the case. A final outcome with healthy TMJ’s and muscles is our goal today.
The phonetic bite registration
As with the previously described muscle-oriented methods, this one begins with muscle relaxation. Then the patient is instructed to speak specific sounds while the anterior teeth are observed by the clinician. Based on the positions assumed by the teeth with specific phonetics, the clinician recognizes the vertical and antero-posterior requirements and records the position, typically also with impression material. Admittedly, this technique requires subjective clinical judgment and the development of a skill without any objective support.
The EMG bite registration
To enhance the precision with which one can determine the optimum muscle-related position, some practitioners recommend monitoring the activity of the masseter, temporalis and anterior digastric muscles electromyographically. Since the electrical muscle output levels involved are just a few microvolts, this measurement requires a high common mode noise rejection amplifier. After relaxation has been verified electromyographically, the patient is instructed to open very gradually until the digastrics show a slight increase in activity (e.g. 0.5 microvolts average). This establishes the limit to which opening the bite is permissible and is typically used as a position for constructing removable orthodontic appliances.
Similar tests are done for closing or repositioning the bite antero-posteriorly while monitoring the elevator muscles. The concept is to find the superior, inferior, anterior and posterior limits of muscle resting. Then the new bite position is selected within these limits. The exact relation chosen may be dependent on many factors, such as clinical findings and the clinician’s best judgment. With this technique it is also possible to evaluate functional activity of the musculature with the bite registration in place to further evaluate the appropriateness of the new maxillo-mandibular relation.

Figure.4. JT-3D Jaw Tracker used together with EMG to monitor a bite registration
The instrument monitored bite registration
To maximize the precision with which one can determine the bite registration position, clinicians can actively monitor the position of the mandible using a magnetic jaw tracker while simultaneously recording EMG activity. After the muscles are relaxed, a recording is made of the movement from rest to centric occlusion, light tapping in CO and protrusive guidance. Next, the registration position is selected and targeted on the computer screen. The treatment position chosen can reflect all of the information available regarding the patient’s current condition. Finally, the registration material is placed in the mouth and the patient is instructed to close into it while the position of the mandible and the muscle activities are monitored on the computer screen. (Figure 5). This allows the clinician to immediately see the three-dimensional relationship between the old centric occlusal position and the new bite position. The saved recording can be recalled later and utilized to evaluate an appliance, provisional restorations or the prosthesis at try-in.
The position of the bite registration and the levels of muscle activity, are simultaneously visible in this combined EMG and jaw tracking recording, as shown in Figure 5. The vertical dimension is increased 2.5 millimetres, the freeway space is reduced from 4.1 mm to 1.6 mm.
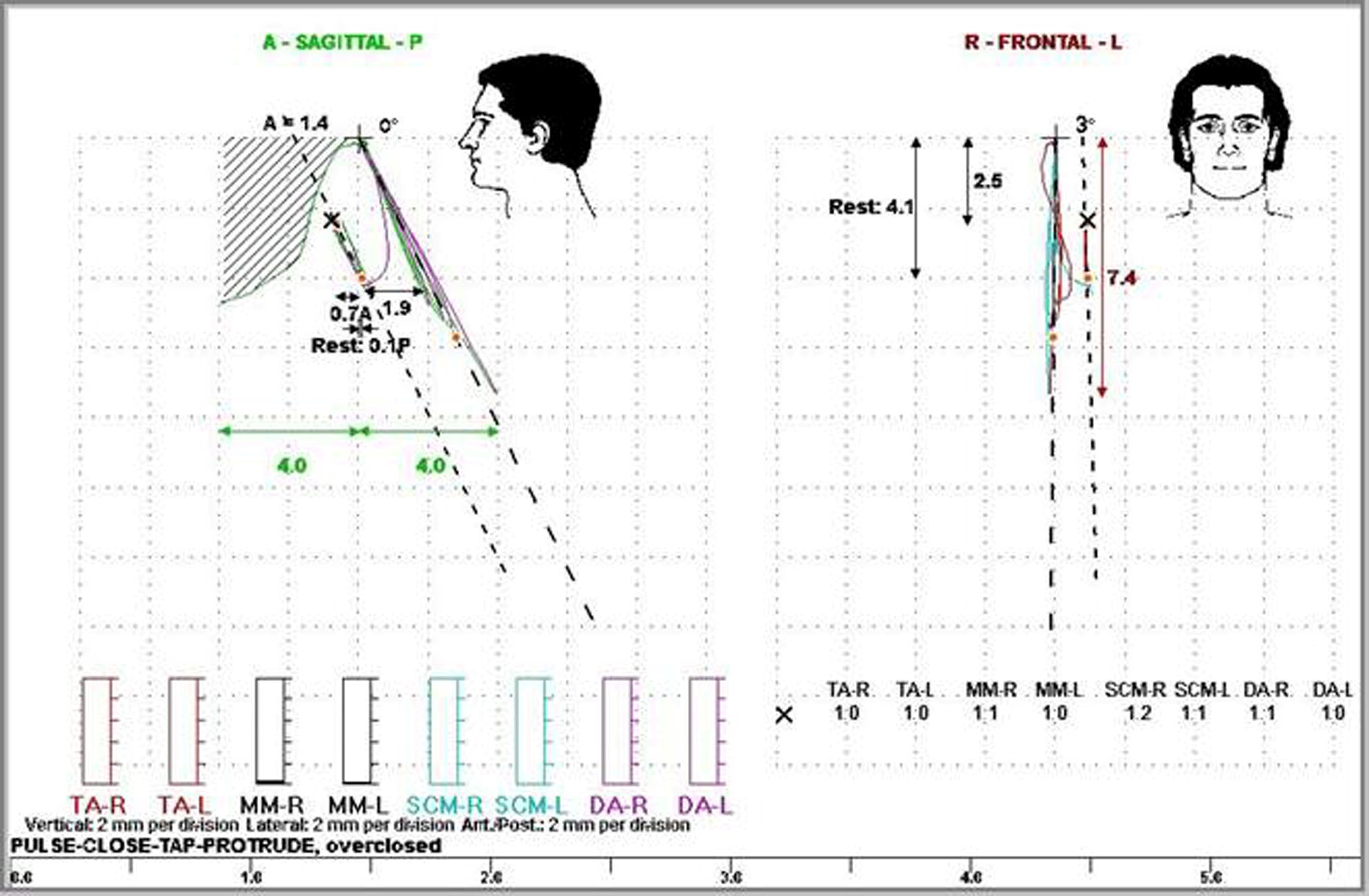
Figure 5. The position of the bite registration and the levels of muscle activity, are simultaneously visible in this combined EMG and jaw tracking recording. The vertical dimension is increased 2.5 millimetres, the freeway space is reduced from 4.1 mm to 1.6 mm.

Figure 6. Example of a patient with an overclosed vertical dimension, due to previous loss of teeth, that has been successfully treated using Neuromuscular Principles.
Predicting a patient’s response to correcting overclosure
The question is often asked, “How quickly will a patient adapt to a new bite registration?” Even though the object is to “correct” a mal-relationship of the mandible to the maxilla, the patient’s current relationship still has familiarity. The new relationship, no matter how “perfectly” established, will seem strange to the patient at first. There are many factors that influence a patient’s adaptation to a new maxillo-mandibular relation. It is possible to estimate a patient’s response by considering the following factors:
- The age of the patient [younger = more adaptive, older = less adaptive]
- The amount of the change [a big change is more difficult to adapt to than a small change]
- The duration of the overclosed condition [a long-standing condition will be more difficult to “de-program” than one of short duration]
- The quality of bilateral TM joint function [good joint function makes adaptation easier]
- An overclosed bite, due to developmental abnormalities (if caught early) can be corrected easily and with rapid adaptation by the patient [children are much more adaptive]
- Overclosure resulting from parafunction typically coincides with a strong, healthy musculature. Strong, healthy muscles make adaptation easier, but require a treatment plan to protect the restored occlusion from destructive parafunctional forces.
- An overclosed bite due to caries, loss of teeth, etc. without evidence of parafunction, typically coincides with a weak musculature, making adaptation difficult. This is very often the case with complete removable prosthetics.
References:
- Costen JB: A syndrome of ear and sinus symptoms dependent upon disturbed function of the temporomandibular joint. Ann Otol Rhin and Laryngol 1934 Mar; 43:1-152
- Costen JB: Glossodynia: Reflex irritation from the mandibular joint as the principal etiologic factor. Arch Otolaryg 1935 Nov;22:554-564
- Costen JB: Neuralgias and ear symptoms. J Am Med Assn 1936 Jul;107:252-255
- Thompson JR: Concepts regarding the function of the stomatognathic system. JADA 1954 Jun; 48:626-637
- Sears VH: Occlusal Pivots. J Prosthet Dent 1956 6:332-338
- Gourion GR. [A new occlusal concept: myocentric relation and the Myo-monitor] Rev Fr Odontostomatol. 1971 Oct;18(8):995-1004. French.
- Fujii H, Mitani H. Reflex responses of the masseter and temporal muscles in man. J Dent Res. 1973 Sep-Oct;52(5):1046-50
- Vesanen E, Vesanen R. The Jankelson Myo-Monitor and its clinical use. Proc Finn Dent Soc. 1973 Dec;69(6):244-7.
- Wessberg GA, Dinham R. The Myo-Monitor and the Myofacial Pain Dysfunction Syndrome. J Hawaii Dent Assoc. 1977 Aug;10(2):10-3.
- Jankelson B, Radke JC. The myo-monitor: its use and abuse (I). Quintessence Int. 1978 Feb;9(2):47-52.
- Jankelson B, Radke JC. The Myo-monitor: its use and abuse (II). Quintessence Int. 1978 Mar;9(3):35-9.
- Kobayashi Y, Nakano Y, Komatsu Y, Ando N. [Clinical study of Myo-monitor. Part 1. An evaluation in the treatment of dysfunction of the masticatory system] 1978 Dec;66(4):539-47. Japanese.
- Rogers Patient’s facial pain treated by Myo-monitor and dentures. Dent Surv. 1979 May;55(5):54.
- Gernet W, Reither W, Gilde H. [Use of the Myo-Monitor in the functionally disturbed stomatognathic system] Dtsch Zahnarztl Z. 1980 Jun;35(6):595-8. German.
- Shen WW. [A study of the myo-monitor and its clinical application] Zhonghua Kou Qiang Ke Za Zhi. 1982 Dec;17(4):193-6. Chinese.
- Yoshida M, Higashi H, Yamauchi M, Takigawa H, Murakami M, Kawano J. [Effect of Myo-monitor pulsing on jaw opening in patients with trismus] Gifu Shika Gakkai Zasshi. 1983 Aug;11(1):157-69. Japanese.
- Dinham Myocentric. A clinical appraisal. Angle Orthod. 1984 Jul;54(3):211-7.
- Boschiero R, Fraccari F, Pagnacco O. [Analysis of the results of using the Myo-Monitor on patients with a reduced mouth opening] Minerva Stomatol. 1986 Sep;35(9):857-64
- Allgood JP. Transcutaneous electrical neural stimulation (TENS) in dental practice. Compend Contin Educ Dent 1986 Oct;7(9):640, 642-4
- Bremerich A, Wiegel W, Thein T, Dietze T. Transcutaneous electric nerve stimulation (TENS) in the therapy of chronic facial pain. Preliminary report. J Craniomaxillofac Surg 1988 Nov;16(8):379-81
- Donegan SJ, Carr AB, Christensen LV, Ziebert GJ. An electromyographic study of aspects of ‘deprogramming’ of human jaw muscles. J Oral Rehabil 1990 Nov;17(6):509-18
- Gomez CE, Christensen Stimulus-response latencies of two instruments delivering transcutaneous electrical neuromuscular stimulation (TENS). J Oral Rehabil 1991 Jan;18(1):87-94
- Carr AB, Donegan SJ, Christensen LV, Ziebert GJ. An electrognathographic study of aspects of ‘deprogramming’ of human jaw muscles. J Oral Rehabil 1991 Mar;18(2):143-8
- Michelotti A, Farella M, Vollaro S, Martina R. Mandibular rest position and electrical activity of the masticatory muscles. J Prosthet Dent. 1997 Jul;78(1):48-53
- Rilo B, Santana U, Mora MJ, Cadarso CM. Myoelectrical activity of clinical rest position and jaw muscle activity in young adults. J Oral Rehabil. 1997 Oct;24(10):735-40
- Sgobbi de Faria CR, Berzin F. Electromyographic study of the temporal, masseter and suprahyoid muscles in the mandibular rest position. J Oral Rehabil 1998 Oct;25(10):776-80
- Eble OS, Jonas IE, Kappert HF. [Transcutaneous electrical nerve stimulation (TENS): its short-term and long-term effects on the masticatory muscles.] J Orofac Orthop 2000;61(2):100-11 [Article in English, German]
- Kamyszek G, Ketcham R, Garcia R Jr, Radke J. Electromyographic evidence of reduced muscle activity when ULF-TENS is applied to the Vth and VIIth cranial nerves. Cranio 2001 Jul;19(3):162-8
- Bessette RW, Quinlivan JT. Electromyographic evaluation of the Myo-Monitor. J Prosthet Dent. 1973 Jul;30(1):19-24.
- Remien JC 2nd, Ash M Jr. “Myo-Monitor centric”: an evaluation. J Prosthet Dent. 1974 Feb;31(2):137-45.
- Noble WH. Anteroposterior position of “Myo-Monitor centric”. J Prosthet Dent. 1975 Apr;33(4):398-402.
32. Azarbal M. Comparison of Myo-Monitor centric position to centric relation and centric occlusion. J Prosthet Dent. 1977 Sep;38(3):331-7.
PO Box 2345, Parramatta NSW 1750 Australia
T: 1800 118 991
E: editor@thedentalreview.com.au







