This article deals with practical oral care for people with intellectual disability. Providing oral care to people with intellectual disability requires adaptation of the skills you use every day. In fact, most people with mild or moderate intellectual disability can be treated successfully in the general practice setting. This article will help you make a difference in the lives of people who need professional oral care.
Intellectual disability is a disorder of mental and adaptive functioning, meaning that people who are affected are challenged by the skills they use in everyday life. Intellectual disability is not a disease or a mental illness; it is a developmental disability that varies in severity and is usually associated with physical problems. While one person with intellectual disability may have slight difficulty thinking and communicating, another may face major challenges with basic self-care and physical mobility.
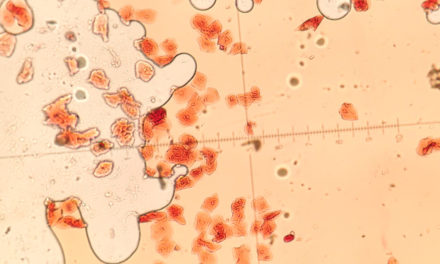
Data indicate that people with intellectual disability have more untreated caries and a higher prevalence of gingivitis and other periodontal diseases than the general population.
Health challenges in intellectual disability and strategies for care
Many people with intellectual disability also have other conditions such as cerebral palsy, seizure or psychiatric disorders, attention deficit/hyperactivity disorder, or problems with vision, communication, and eating. Though language and communication problems are common in anyone with intellectual disability, motor skills are typically more affected when a person has coexisting conditions.
Before the appointment, obtain and review the patient’s medical history. Consultation with physicians, family, and caregivers is essential to assembling an accurate medical history. Also, determine who can legally provide informed consent for treatment.
Mental challenges
People with intellectual disability learn slowly and often with difficulty. Ordinary activities of daily living, such as brushing teeth and getting dressed, and understanding the behaviour of others as well as their own, can all present challenges to a person with intellectual disability.
- Set the stage for a successful visit by involving the entire dental team–from the receptionist’s friendly greeting to the caring attitude of the dental assistant in the operatory. All should be aware of your patient’s mental challenges.
- Reduce distractions in the operatory, such as unnecessary sights, sounds, or other stimuli, to compensate for the short attention spans commonly observed in people with intellectual disability.
- Talk with the parent or caregiver to determine your patient’s intellectual and functional abilities, then explain each procedure at a level the patient can understand. Allow extra time to explain oral health issues or instructions and demonstrate the instruments you will use.
- Address your patient directly and with respect to establish a rapport. Even if the caregiver is in the room, direct all questions and comments to your patient.
- Use simple, concrete instructions and repeat them often to compensate for any short-term memory problems. Speak slowly and give only one direction at a time.
- Be consistent in all aspects of oral care, since long-term memory is usually unaffected. Use the same staff and dental operatory each time to help sustain familiarity. The more consistency you provide for your patients, the more likely they will cooperate.
- Listen actively, since communicating clearly is often difficult for people with intellectual disability. Show your patient whether you understand. Be sensitive to the methods he or she uses to communicate, including gestures and verbal or nonverbal requests.
Behaviour challenges
While most people with intellectual disability do not pose significant behaviour problems that complicate oral care, anxiety about dental treatment occurs frequently. People unfamiliar with a dental office and its equipment and instruments may exhibit fear. Some react to fear with uncooperative behaviour, such as crying, wiggling, kicking, aggressive language, or anything that will help them avoid treatment. You can make oral health care a better experience by comforting your patients and acknowledging their anxiety.
- Talk to the caregiver or physician about techniques they have found to be effective in managing the patient’s behaviour.
- Schedule patients with intellectual disability early in the day if possible. Early appointments can help ensure that everyone is alert and attentive and that waiting time is reduced.
- Keep appointments short and postpone difficult procedures until after your patient is familiar with you and your staff.
- Allow extra time for your patients to get comfortable with you, your office, and the entire oral health care team. Invite patients and their families to visit your office before beginning treatment.
- Permit the parents or caregiver to come into the treatment setting to provide familiarity, help with communication, and offer a calming influence by holding your patient’s hand during treatment. Some patients’ behaviour may improve if they bring comfort items such as a stuffed animal or blanket.
- Reward cooperative behaviour with compliments throughout the appointment.
- Consider nitrous oxide/oxygen sedation to reduce anxiety and fear and improve cooperation. Obtain informed consent from the legal guardian before administering any kind of sedation.
- Use immobilization techniques only when absolutely necessary to protect the patient and staff during dental treatment–not as a convenience. There are no universal guidelines on immobilization that apply to all treatment settings. Before employing any kind of immobilization, it may help to consult available guidelines on federally funded care, your State department of mental health/disabilities, and your State Dental Practice Act. Guidelines on behaviour management published by the American Academy of Paediatric Dentistry may also be useful. Obtain consent from your patient’s legal guardian and choose the least restrictive technique that will allow you to provide care safely. Immobilization should not cause physical injury or undue discomfort.
People with intellectual disability often engage in perseveration, a continuous, meaningless repetition of words, phrases, or movements. Your patient may mimic the sound of the suction, for example, or repeat an instruction over and again. Avoid demonstrating dental equipment if it triggers perseveration, and note this in the patient’s record.
Physical challenges
Intellectual disability does not always include a specific physical trait, although many people have distinguishing features such as orofacial abnormalities, scoliosis, unsteady gait, or hypotonia due to coexisting conditions. Countering physical challenges requires attention to detail.
- Maintain clear paths for movement throughout the treatment setting. Keep instruments and equipment out of the patient’s way.
- Place and maintain your patient in the centre of the dental chair to minimize the risk of injury. Placing pillows on both sides of the patient can provide stability.
- If you need to transfer your patient from a wheelchair to the dental chair, ask the patient or caregiver about special preferences such as padding, pillows, or other things you can provide to ease the transition. The patient or caregiver can often explain how to make a smooth transfer.
- Some patients cannot be moved into the dental chair but instead must be treated in their wheelchairs. Some wheelchairs recline or are specially moulded to fit people’s bodies. Lock the wheels, then slip a sliding board (also called a transfer board) behind the patient’s back to provide support for the head and neck during care.
Cereal palsy occurs in one-fourth of those who have intellectual disability and tends to affect motor skills more than cognitive skills. Uncontrolled body movements and reflexes associated with cerebral palsy can make it difficult to provide care.
- Place and maintain your patient in the centre of the dental chair. Do not force arms and legs into unnatural positions, but allow your patient to settle into a position that is comfortable and will not interfere with dental treatment.
- Observe your patient’s movements and look for patterns to help you anticipate direction and intensity. Trying to stop these movements may only intensify the involuntary response. Try instead to anticipate the movements, blending your movements with those of your patient or working around them.
- Softly cradle your patient’s head during treatment. Be gentle and slow if you need to turn the patient’s head.
- Help minimize the gag reflex by placing your patient’s chin in a neutral or downward position.
- Stay alert and work efficiently in short appointments.
- Exert gentle but firm pressure on your patient’s arm or leg if it begins to shake.
- Take frequent breaks or consider prescribing muscle relaxants when long procedures are needed. People with cerebral palsy may need sedation, general anaesthesia, or hospitalization if extensive dental treatment is required.
Cardiovascular anomalies such as heart murmurs and damaged heart valves occur frequently in people with intellectual disability, especially those with Down syndrome or multiple disabilities. Consult the patient’s physician to determine if antibiotic prophylaxis is necessary for dental treatment.
Seizures are common in this population but can usually be controlled with anticonvulsant medications. The mouth is always at risk during a seizure: Patients may chip teeth or bite the tongue or cheeks. Persons with controlled seizure disorders can easily be treated in the general dental office.
- Consult your patient’s physician. Record information in the chart about the frequency of seizures and the medications used to control them. Determine before the appointment whether medications have been taken as directed. Know and avoid any factors that trigger your patient’s seizures.
- Be prepared to manage a seizure. If one occurs during oral care, remove any instruments from the mouth and clear the area around the dental chair. Attaching dental floss to rubber dam clamps and mouth props when treatment begins can help you remove them quickly. Do not attempt to insert any objects between the teeth during a seizure.
- Stay with your patient, turn him or her to one side, and monitor the airway to reduce the risk of aspiration.
Visual impairments, most commonly strabismus (crossed or misaligned eyes) and refractive errors, can be managed with careful planning.
- Determine the level of assistance your patient requires to move safely through the dental office.
- Use your patients’ other senses to connect with them, establish trust, and make treatment a good experience. Tactile feedback, such as a warm handshake, can make your patients feel comfortable.
- Face your patients when you speak and keep them apprised of each upcoming step, especially when water will be used. Rely on clear, descriptive language to explain procedures and demonstrate how equipment might feel and sound. Provide written instructions in large print (16 point or larger).
Hearing loss and deafness can also be accommodated with careful planning. Patients with a hearing problem may appear to be stubborn because of their seeming lack of response to a request.
- Patients may want to adjust their hearing aids or turn them off, since the sound of some instruments may cause auditory discomfort.
- If your patient reads lips, speak in a normal cadence and tone. If your patient uses a form of sign language, ask the interpreter to come to the appointment. Speak with this person in advance to discuss dental terms and your patient’s needs.
- Visual feedback is helpful. Maintain eye contact with your patient. Before talking, eliminate background noise (turn off the radio and the suction). Sometimes people with a hearing loss simply need you to speak clearly in a slightly louder voice than normal. Remember to remove your facemask first or wear a clear face shield.
Record in the patient’s chart strategies that were successful in providing care. Note your patient’s preferences and other unique details that will facilitate treatment, such as music, comfort items, and flavour choices
Oral health problems in intellectual disability and strategies for care
In general, people with intellectual disability have poorer oral health and oral hygiene than those without this condition. Data indicate that people who have intellectual disability have more untreated caries and a higher prevalence of gingivitis and other periodontal diseases than the general population.
Periodontal disease
Medications, malocclusion, multiple disabilities, and poor oral hygiene combine to increase the risk of periodontal disease in people with intellectual disability.
- Encourage independence in daily oral hygiene. Ask patients to show you how they brush, and follow up with specific recommendations on brushing methods or toothbrush adaptations. Involve your patients in hands-on demonstrations of brushing and flossing.
- Some patients cannot brush and floss independently due to impaired physical coordination or cognitive skills. Talk to their caregivers about daily oral hygiene. Do not assume that all caregivers know the basics; demonstrate proper brushing and flossing techniques. A power toothbrush or a floss holder can simplify oral care. Also, use your experiences with each patient to demonstrate sitting or standing positions for the caregiver. Emphasize that a consistent approach to oral hygiene is important–caregivers should try to use the same location, timing, and positioning.
- Some patients benefit from the daily use of an antimicrobial agent such as chlorhexidine. Recommend an appropriate delivery method based on your patient’s abilities. Rinsing, for example, may not work for a patient who has swallowing difficulties or one who cannot expectorate. Chlorhexidine applied using a spray bottle or toothbrush is equally efficacious.
- If use of particular medications has led to gingival hyperplasia, emphasize the importance of daily oral hygiene and frequent professional cleanings.
Dental caries
People with intellectual disability develop caries at the same rate as the general population. The prevalence of untreated dental caries, however, is higher among people with intellectual disability, particularly those living in noninstitutionalised settings.
- Emphasize non-cariogenic foods and beverages as snacks. Advise caregivers to avoid using sweets as incentives or rewards.
- Advise patients taking medicines that cause xerostomia to drink water often. Suggest sugar-free medicine if available and stress the importance of rinsing with water after dosing.
- Recommend preventive measures such as fluorides and sealants.
Malocclusion
The prevalence of malocclusion in people with intellectual disability is similar to that found in the general population, except for those with coexisting conditions such as cerebral palsy or Down syndrome. A developmental disability in and of itself should not be perceived as a barrier to orthodontic treatment. The ability of the patient or caregiver to maintain good daily oral hygiene is critical to the feasibility and success of treatment.
Missing permanent teeth, delayed eruption and enamel hypoplasia
Missing permanent teeth, delayed eruption and enamel hypoplasia are more common in people with intellectual disability and coexisting conditions than in people with intellectual disability alone.
- Examine a child by his or her first birthday and regularly thereafter to help identify unusual tooth formation and patterns of eruption.
- Consider using a panoramic radiograph to determine whether teeth are congenitally missing. Patients often find this technique less threatening than individual films.
- Take appropriate steps to reduce sensitivity and risk of caries in your patients with enamel hypoplasia
Damaging oral habits
Damaging oral habits are a problem for some people with intellectual disability. Common habits include bruxism; mouth breathing; tongue thrusting; self-injurious behaviour such as picking at the gingiva or biting the lips; and pica, eating objects and substances such as gravel, cigarette butts, or pens. If a mouth guard can be tolerated, prescribe one for patients who have problems with self-injurious behaviour or bruxism
Trauma and injury
Trauma and injury to the mouth from falls or accidents occur in people with intellectual disability. Suggest a tooth-saving kit for group homes. Emphasize to caregivers that traumas require immediate professional attention and explain the procedures to follow if a permanent tooth is knocked out. Also, instruct caregivers to locate any missing pieces of a fractured tooth, and explain that radiographs of the patient’s chest may be necessary to determine whether any fragments have been aspirated.
Physical abuse often presents as oral trauma. Abuse is reported more frequently in people with developmental disabilities than in the general population. If you suspect that a child is being abused or neglected, State laws require that you call your Child Protective Services agency.
Making a difference in the oral health of a person with intellectual disability may go slowly at first, but determination can bring positive results–and invaluable rewards. By adopting the strategies discussed in this booklet, you can have a significant impact not only on your patients’ oral health, but on their quality of life as well.
Reproduced February 2017 from NIH Publication No. 09-5194